Publication: CTLA-4-expressing ILC3s restrain interleukin-23-mediated inflammation
Published in: Nature, 2024, 630 (8018), pp.976-983. ⟨10.1038/s41586-024-07537-3⟩
Authors: Anees Ahmed, Ann M Joseph, Jordan Zhou, Veronika Horn, Jazib Uddin, Mengze Lyu, Jeremy Goc, David Artis, Randy Longman, Gregory F Sonnenberg, Ellen Scherl, Robbyn E Sockolow, Dana Lukin, Vinita Jacob, Laura Sahyoun, Michael Mintz, Lasha Gogokhia, Thomas Ciecierega, Aliza Solomon, Arielle Bergman, Kimberley Chein, Elliott Gordon, Michelle Ramos, Victoria Ribeiro de Godoy, Adriana Brcic-Susak, Seun Oguntunmibi, Dario Garone, Caitlin Mason, Robbyn E Sockolow, James B Wing, Eric Vivier, Shimon Sakaguchi, Gregory F Sonnenberg
Summary
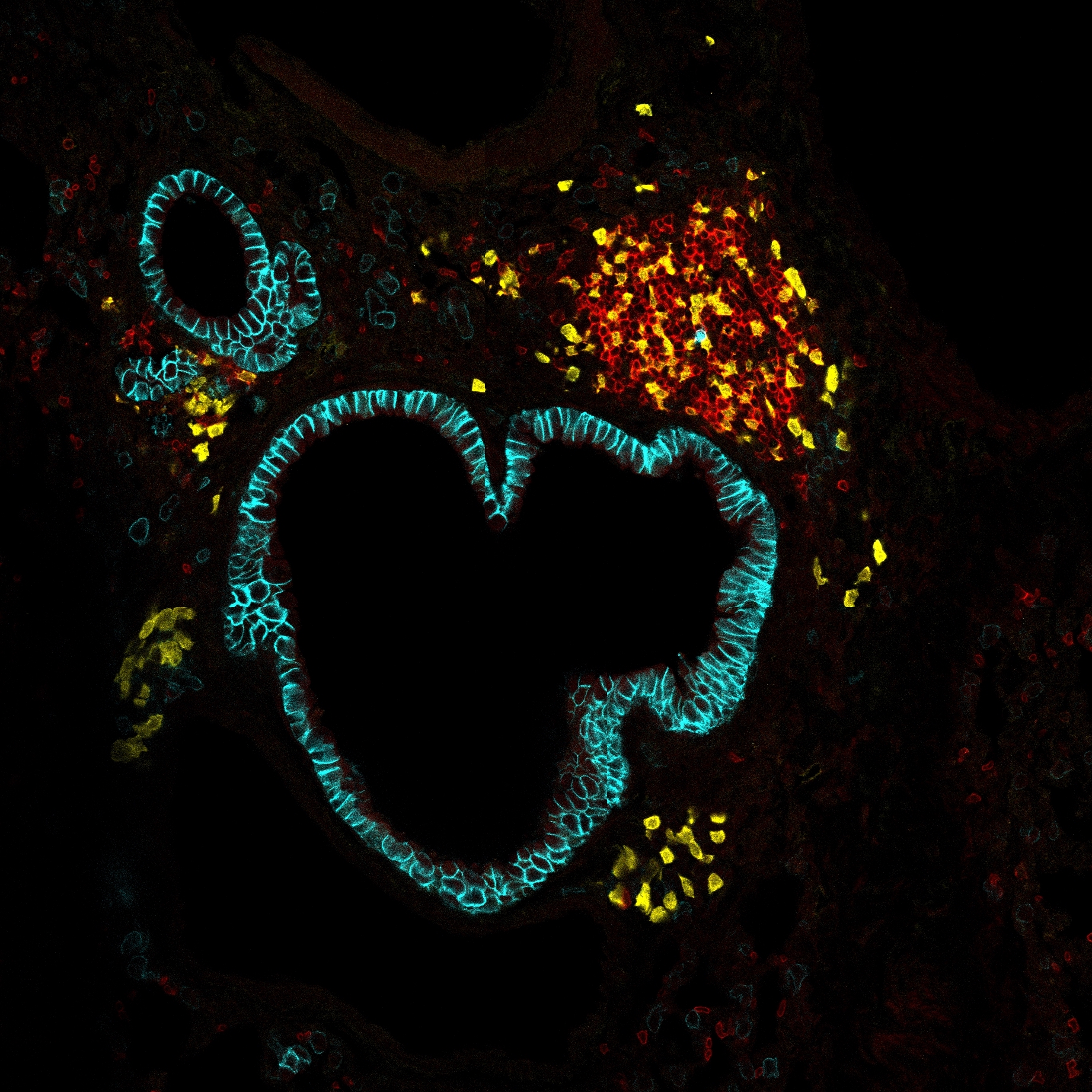
Interleukin (IL-)23 is a major mediator and therapeutic target in chronic inflammatory diseases, that also elicits tissue-protection in the intestine at homeostasis or following acute infection 1-4 . However, the mechanisms shaping these beneficial versus pathologic outcomes remain poorly understood. To address this gap in knowledge, we performed single cell RNA-sequencing on all IL-23 receptor expressing cells in the intestine and their acute response to IL-23, revealing a dominance of T cells and group 3 innate lymphoid cells (ILC3s). Unexpectedly, we identified potent upregulation of the immunoregulatory checkpoint molecule, cytotoxic T-lymphocyteassociated antigen-4 (CTLA-4), on ILC3s. This pathway was activated by gut microbes and IL-23 in a FOXO1-and STAT3-dependent manner. Mice lacking CTLA-4 on ILC3s exhibit reduced regulatory T cells, elevated inflammatory T cells, and more severe intestinal inflammation. IL-23 induction of CTLA-4 + ILC3s was necessary and sufficient to reduce co-stimulatory molecules and increase PD-L1 bioavailability on intestinal myeloid cells. Finally, human ILC3s upregulate CTLA-4 in response to IL-23 or gut inflammation and correlate with immune regulation in inflammatory bowel disease (IBD). These results reveal ILC3-intrinsic CTLA-4 as an essential checkpoint that restrains the pathologic outcomes of IL-23, suggesting that disruption of these lymphocytes, which occurs in IBD 5-7 , contributes to chronic inflammation. IL-23 is a heterodimeric cytokine belonging to the IL-12 family, encompassing a shared IL-12p40 subunit and specific IL-23p19 subunit 1,8,9 . Basic mouse models, genetic studies in patients, and clinical trials identified that IL-23 is a major mediator of autoimmune and chronic inflammatory disorders, including inflammatory bowel disease (IBD) 9 , psoriasis 10 , rheumatoid arthritis 11 , and multiple sclerosis 12 . For example, genome-wide association studies identified single-nucleotide polymorphisms in IL-23 receptor (IL-23R) loci that strongly associate with disease pathogenesis 13,14 , and blocking IL-23 provides therapeutic benefit in a subset of patients 15-17 . However, IL-23 exhibits numerous beneficial, antimicrobial, and tissue protective functions. This is particularly evident in the intestine, where IL-23 is produced in response to microbiota colonization, and blockade of IL-23 alters microbiota composition 18 , increases susceptibility to enteric infections 19-21 , or in some cases exacerbates gut inflammation 22,23 . Further, humans with loss-of-function mutations in IL23R are more susceptible to various bacterial and fungal infections at mucosal surfaces 24 . This creates a paradigm that IL-23 mediates both tissue protective and pathologic responses, particularly in the intestine, but the cellular and molecular mechanisms controlling these disparate outcomes remains unclear.
Link to HAL – amu-04934644
Link to DOI – 10.1038/s41586-024-07537-3