Publication: The Association of Low CD4 Expression on Monocytes and Low CD8+ T-Cell Count at Hospital Admission Predicts the Need for Mechanical Ventilation in Patients With COVID-19 Pneumonia: A Prospective Monocentric Cohort Study.
Published in: Crit Care Explor 2022 Dec; 4(12): e0810
Authors: Allardet-Servent J, Ait Belkacem I, Miloud T, Benarous L, Galland F, Halfon P, Mège JL, Penaranda G, Busnel JM, Malergue F
Summary
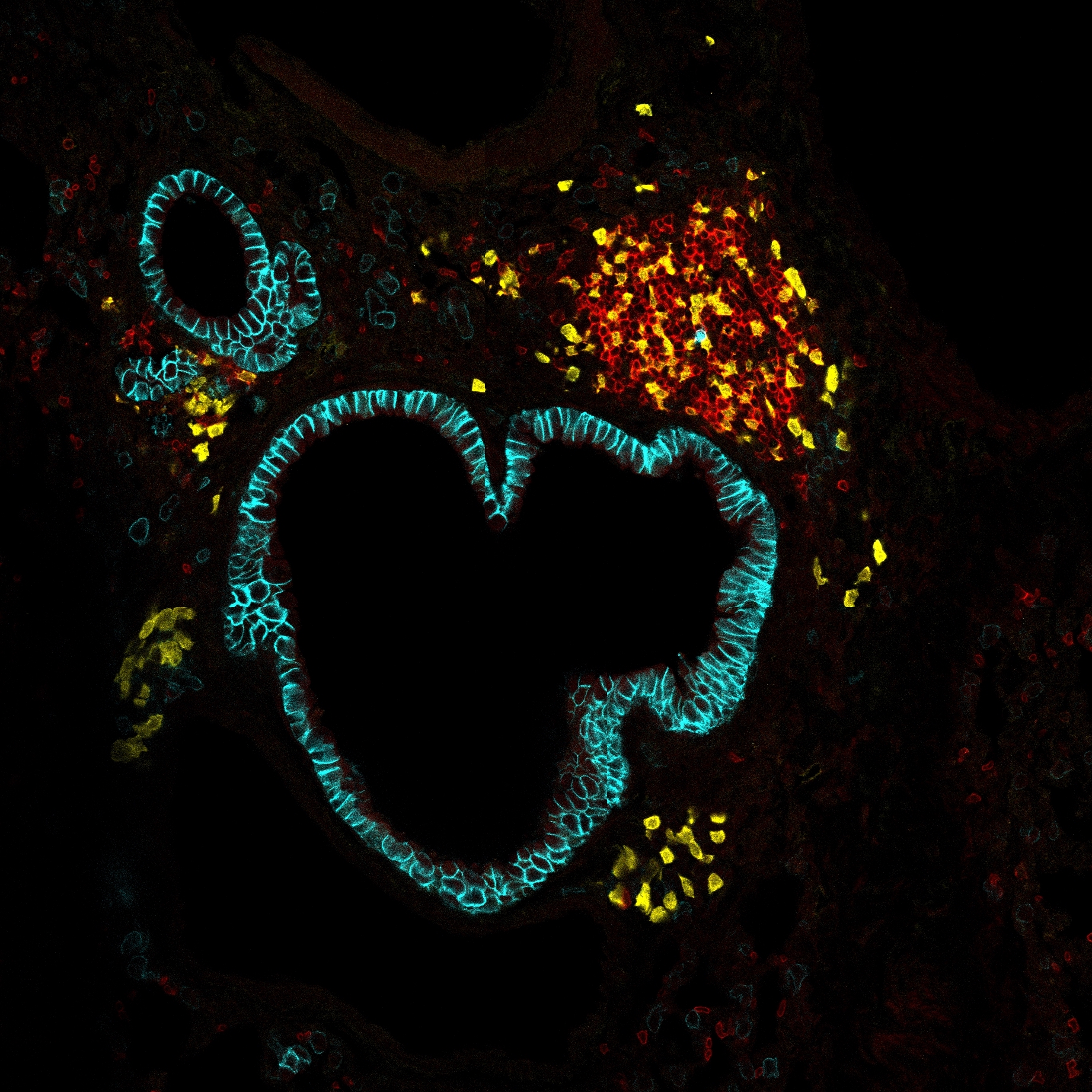
To identify COVID-19-associated immunophenotyping patterns at hospital admission and to determine if some patterns could predict the need for mechanical ventilation (MV).Prospective observational monocentric cohort study.A university-affiliated hospital in Marseille, France.Thirty patients presenting with laboratory-confirmed COVID-19 pneumonia were enrolled within the first 48 hours of hospital admission and compared with 18 healthy controls.None.Whole-blood leukocytes were immunophenotyped with a rapid and simplified one-step flow cytometry method. Thirty-eight immune and five laboratory parameters were compared first between COVID-19 patients and controls and then between the COVID-19 patients who received or not MV during their stays. The variables that significantly discriminated MV from non-MV patients in univariate analysis were entered into a multiple stepwise logistic regression analysis. The COVID-19 patients were predominantly male (87%), aged 61 years (50-71 yr), and 93% received early corticosteroid therapy. Sixteen patients (53%) were managed with noninvasive respiratory support, and 14 (47%) required MV. Compared with controls, COVID-19 patients were characterized by an immune signature featuring: 1) decreased HLA-DR expression on monocytes; 2) reduced basophils, eosinophils, T-cells, NK cells, and nonclassical monocyte count; and 3) up regulation of CD169 on monocytes, CD64 on neutrophils, the adhesion/migration markers (CD62L and CD11b), and the checkpoint inhibitor CD274 on myeloid cells. Among the COVID-19 patients, those who received MV had lower level of CD4 and HLA-DR on monocytes, lower CD8+ T-cell count, and higher lactate dehydrogenase at hospital admission. In multivariate analysis, only CD4 on monocytes (p = 0.032) and CD8+ T-cell count (p = 0.026) were associated with MV requirement. The model combining these two variables provided an area under curve of 0.97 (95% CI, 0.83-0.99).The association of low CD4 on monocytes and low CD8+ T-cell count at hospital admission was highly predictive of the need for MV in hospitalized patients with COVID-19 pneumonia.
Link to Pubmed [PMID] – 36518218
Link to DOI – 10.1097/CCE.0000000000000810
