Publication: B-cell non-Hodgkin lymphoma linked to Coxiella burnetii
Publié dans: Blood, 2016, 127 (1), pp.113-121. ⟨10.1182/blood-2015-04-639617⟩
Auteurs: Clea Melenotte, Matthieu Million, Gilles Audoly, Audrey Gorse, Herve Dutronc, Gauthier Roland, Michal Dekel, Asuncion Moreno, Serge Cammilleri, Maria Patrizia Carrieri, Camelia Protopopescu, Philippe Ruminy, Hubert Lepidi, Bertrand Nadel, Jean-Louis Mege, Luc Xerri, Didier Raoult
Résumé
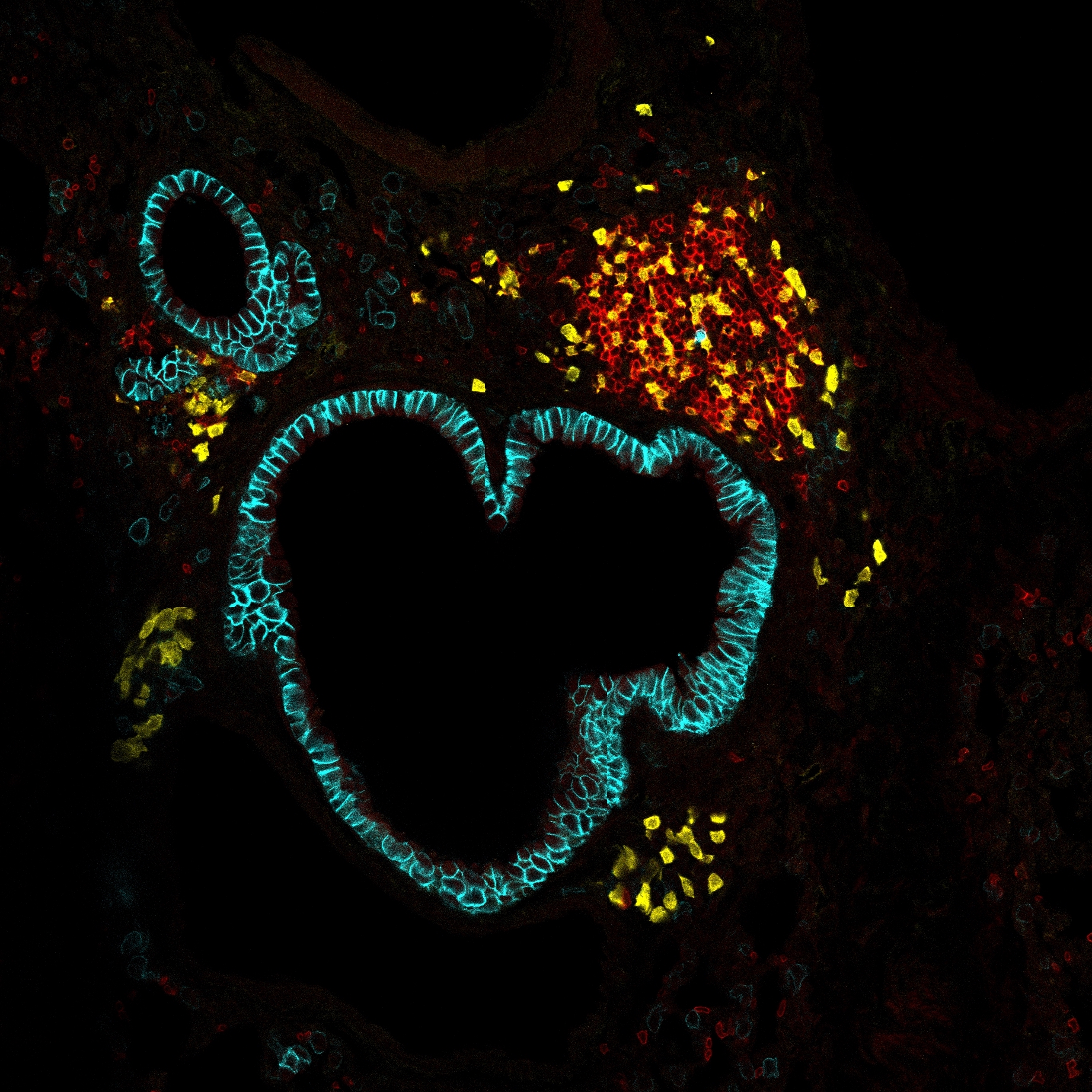
Bacteria can induce human lymphomas, whereas lymphoproliferative disorders have been described in patients with Q fever. We observed a lymphoma in a patient with Q fever that prompted us to investigate the association between the 2 diseases. We screened 1468 consecutive patients of the 2004 to 2014 French National Referral Center for Q fever database. The standardized incidence ratios (SIRs) of diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL) were calculated comparatively to the 2012 Francim Registry. The presence of Coxiella burnetii was tested using immunofluorescence and fluorescence in situ hybridization using a specific 16S ribosomal RNA probe and genomic DNA probe. Seven patients (0.48%) presented mature B-cell lymphoma consisting of 6 DLBCL and 1 FL. An excess risk of DLBCL and FL was found in Q fever patients compared with the general population (SIR [95% confidence interval], 25.4 [11.4-56.4] and 6.7 [0.9-47.9], respectively). C burnetii was detected in CD68(+) macrophages within both lymphoma and lymphadenitis tissues but localization in CD123(+) plasmacytoid dendritic cells (pDCs) was found only in lymphoma tissues. Q fever patients with persistent focalized infection were found more at risk of lymphoma (hazard ratio, 9.35 [1.10-79.4]). Interleukin-10 (IL10) overproduction (P = .0003) was found in patients developing lymphoma. These results suggest that C burnetii should be added to the list of bacteria that promote human B-cell non-Hodgkin lymphoma, possibly by the infection of pDCs and IL10 overproduction. Screening for early lymphoma diagnosis should be considered in the management of patients with Q fever, especially those with persistent focalized infections.
Lien vers Pubmed [PMID] – 26463422
Lien vers HAL – hal-01440249
Lien vers le DOI – 10.1182/blood-2015-04-639617

